Reading the signs of migraines with ML: from algorithm to successful product development
By Desmond Cheung & Roderick Van Den Bergh

Some very common medical conditions like migraine have evaded diagnosis and treatment until now. We explore why Machine Learning might finally be the tool to tame migraines but why it is still not an easy path to a successful product.
Migraines affect 1 in 5 women, but we know little about what causes them, or how to prevent them. Across the EU, the cost of migraines (including direct and indirect costs) has been estimated at €27bn, but nothing can account for the negative impact on quality of life of sufferers and their families.
The complexity of migraines has meant that it has long evaded attempts to help sufferers understand and manage their condition. Early symptoms and triggers can be hard to spot and use of medication at the wrong time can actually worsen a migraine. Layering cutting-edge machine learning techniques on top of medical understanding and advances in sensor technology provide us with an opportunity to finally develop products to manage this and other similar conditions.
Developing an algorithm that can tackle migraines
Whilst we may not fully understand many of the physiological mechanisms in the body, not least those which cause migraines, there is an opportunity to pre-emptively address the condition by monitoring relevant physiological signs, applying modern machine learning (“ML”) techniques and correlating the data collected to how the patient is feeling (patient reported outcomes).
To understand the relevance of ML, consider the following: On one hand, rapidly changing serotonin levels and dilation of cranial blood vessels have been shown to be directly related to migraine attacks. But these signs are challenging to measure and monitor unobtrusively on a continuous basis.
On the other hand, surrogate data such as blood pressure and heart rate are readily collectable, but their physiological links to migraine attacks are indirect. They are also more strongly influenced by other things such as exercise so any changes must be disambiguated from those causes. Hence, it is more difficult to extract useful information about imminent migraine attacks. This is where machine learning can be particularly useful.
Extracting the relationship between the onset of migraine, blood pressure (BP) and heart rate (HR), whilst ignoring the changes in BP and HR due to other factors is almost impossible with conventional rule-based and hand-coded algorithms. Added to this is the challenge of person-to-person variation. So, for best performance, the algorithm must be tuned for each patient. This is really only viable using a machine learning approach.
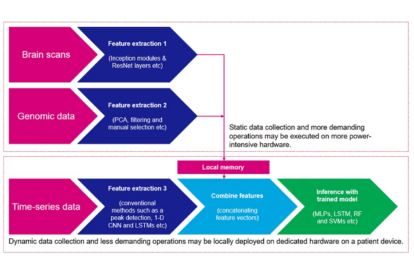
Human data is naturally multimodal and for migraine we consider time series such as: BP, HR(V), ECG and movement. Modern machine learning techniques can handle this data homogeneously with non-time series data: images from MRI’s, written text in medical records and sentiment analysis from voice data. The two types of data are used to create a personalised model that is capable of performing real time inference on the live time series data.
Building a migraine product starts by mocking-up a “draft” model capable of receiving and learning from the appropriate data sources. Using medical domain knowledge and consideration for best practices in explainable-AI we can refine the architecture, and hyper-parameter tuning provides for performance improvement. By benchmarking we can judge the relevance and impact of fidelity of different data sources which allows optimisation of both the data capture and processing. The result is to create a medically valid algorithm. Ultimately, the stratification of patient cohorts becomes an intrinsic feature of the analysis. Precision medicine, using tiered and eventually per-patient generated models, becomes the norm.
For example, we might use the architecture shown below to use the patient profile to tune the general model which is then used for the real time inference.
Although for some applications such as generic speech recognition ML-enabled products have become an off-the-shelf (“OTS”) commodity, applying ML to complex multimodal medical applications such as this is exceptionally non-trivial. Blindly fitting medical data to OTS models, without understanding the underlying physiological drivers is not only wasteful in terms of development time and cost but will also likely face regulatory challenges during product deployment. Instead, applying specialist medical domain knowledge and a deep understanding of the underlying mathematics of ML leads to more efficient and leaner development processes, and ultimately a product with real clinical benefits.
Developing a successful product
It is imperative to remain patient centric! If it is to be valuable, any solution must provide real benefit to patients. Usability must be central to the design and any sensing required must be unobtrusive. The accuracy (sensitivity and specificity) of the algorithm must be useful, and the risks of false positives and negatives must be managed, especially when the administration of a drug is involved. From a business perspective, the solution must be acceptable to the health economic ecosystem and either fit within, or intentionally disrupt existing care pathways.
An enormous challenge is to bridge the gap between rapid innovation and approvable medical device or SaMD. This is because there is risk of a mismatch between the expectations of a non-medical design team and the strictly regulated product development team. Some common gaps which need to be considered (if not addressed) right from the start are:
- Understanding regulatory frameworks and guidance
- User experience and integration into clinical workflows
- Product development practices and quality
Our way to address these challenges is by using design-led innovation and close collaboration between all the relevant stakeholders.
ML provides an opportunity to address some previously unmet patient needs such as migraines. However, multidisciplinary development expertise must be brought to bear throughout algorithm and product development in order to be clinically meaningful and commercially successful in the market.
The application of ML tools in healthcare will also raise ethical challenges, and in a future TTP blog we consider how a multidisciplinary development team may address these to genuinely improve population health outcomes.


